Have you ever wondered how your body fights off infections and diseases?
One of the ways it does so is by developing immunity, which is the ability to resist a specific pathogen or toxin.
There are different types of immunity that your body can acquire, depending on how you encounter the pathogen or toxin.
In this article, we will focus on two types: natural active immunity and acquired passive immunity.
Natural Active Immunity: What It Is and Why It Matters
Natural active immunity occurs when you are exposed to a live pathogen through natural infection
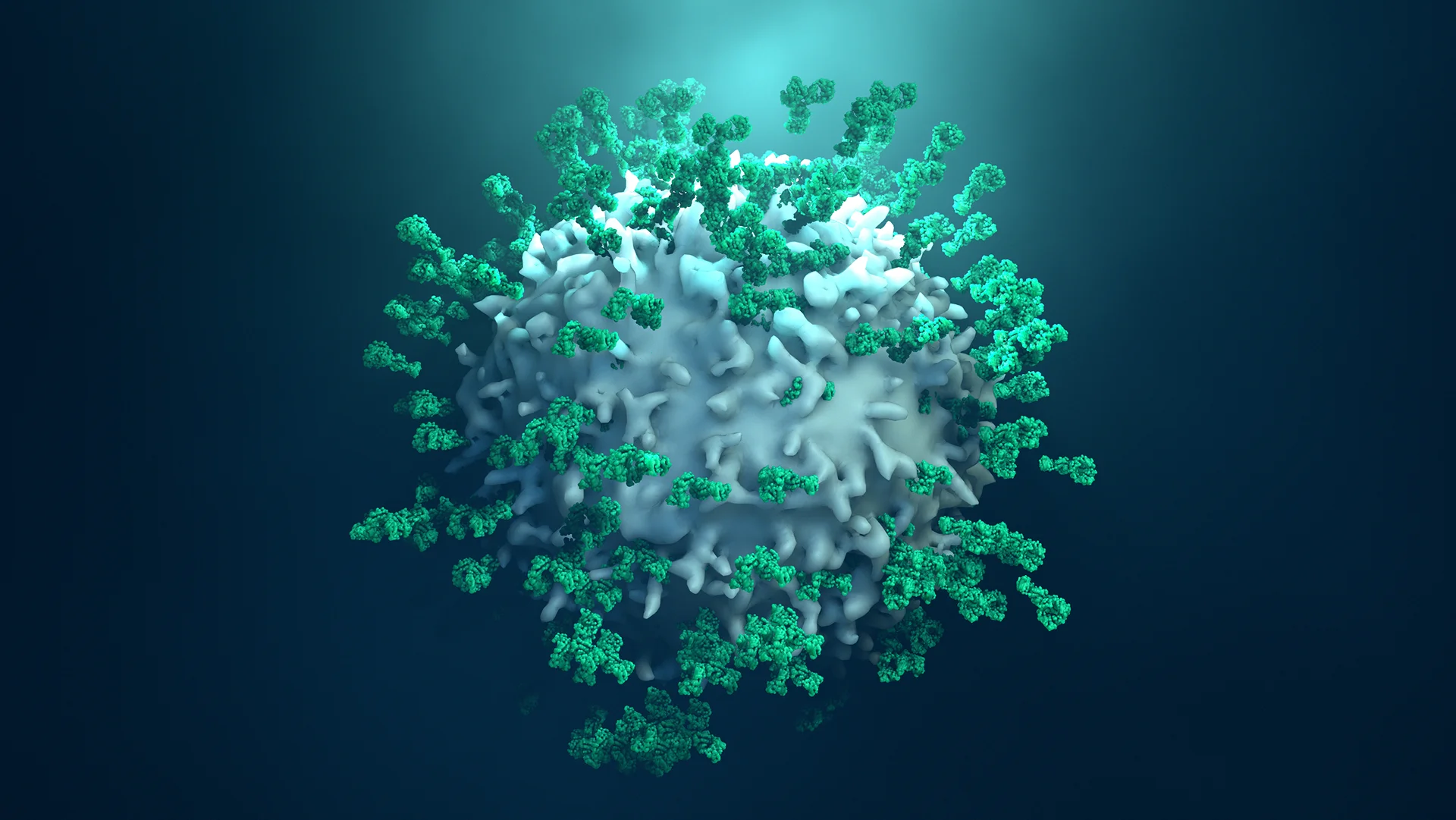
Your immune system recognizes the pathogen as foreign and produces antibodies that bind to and neutralize it.
Antibodies are proteins that help attack pathogens, such as bacteria and viruses.
The process of producing antibodies takes time, so you may still get sick from the infection.
However, some of the antibodies remain in your body after you recover, giving you long-lasting protection against future infections by the same pathogen.
This is why you usually don’t get chickenpox or measles more than once in your lifetime.
Passive Immunity
Acquired passive immunity occurs when you receive antibodies from another source rather than producing them yourself.
For example, a newborn baby acquired passive immunity from its mother through the placenta or breast milk.
Another example is immunoglobulin treatments, which are antibody-containing blood products that may be given to people at risk for infections.
Acquired passive immunity provides immediate but short-term protection against infection because the antibodies eventually break down and leave your body.
Both natural active immunity and acquired passive immunity are important for health and disease prevention because they help your body fight off pathogens that could cause serious illness or death.
Some examples of diseases that can be prevented by these types of immunity are tetanus, rabies, hepatitis B, measles, mumps, rubella, chickenpox, polio, diphtheria and whooping cough.
Active vs. Passive Immunity

When it comes to immunity, there are two main types – natural active immunity and artificially acquired (or passive) immunity.
Let’s look into their differences.
Natural active immunity is when your body produces its own antibodies that recognize and destroy foreign substances in your body without any outside help or medical interventions.
Natural active immunity is long-lasting because once your immune system recognizes a particular invader it will remember it for years and create an appropriate response if it ever encounters it again.
This form of immunity may also be weakened due to poor nutrition or latest virus infections like SARS-CoV2 which affects the way the immune system functions.
Artificially acquired (or passive) immunities can occur when someone ingests antibodies created in lab through injections or consuming products like vaccines with dead or inactivated pathogens they were made from.
Passive immunity only lasts a certain period of time because once we consume this type of antibody, our bodies tend to get rid of them quickly due to the fact that our bodies can’t tell apart what was within the injection/vaccine compared to anything naturally occurring within usᅳthus resulting in their quick elimination from our systems by purging them out via urine or through bile acids produced by liver cells.
Examples of Active and Passive Immunity
Natural active immunity is evident when a baby is born, having developed their own immune system from birth.
Someone who contracts and recovers from the flu will have developed natural immunity to that specific strain of the virus.
Artificially acquired (passive) immunities are obtained through vaccination against diseases like hepatitis or chickenpox.
In these cases, the individual is injected with antibodies containing dead or inactive pathogen particles that do not cause any harm. These particles teach the body to respond properly to the specific germs upon further encounters, preventing infection from those diseases.
Examples of such vaccines include the flu vaccine, the measles-mumps-rubella (MMR) vaccine, and the COVID-19 vaccine.
Limitations of Active and Passive Immunity
However, natural active immunity and acquired passive immunity have some limitations.
Natural active immunity depends on exposure to a live pathogen which can be dangerous or fatal for some people.
Acquired passive immunity depends on availability of antibody sources which can be scarce or expensive for some people.
Moreover neither type of immunity protects against all pathogens because different pathogens require different antibodies.
Therefore one way to enhance your immune system is by getting vaccinated.
Vaccination is a form of active immunization which involves introducing a killed or weakened form of a pathogen into your body.
This stimulates your immune system to produce antibodies without causing disease symptoms.
Vaccination gives you long-term protection against many diseases without exposing you to harmful pathogens or relying on external sources of antibodies.
Natural active immunity and acquired passive immunity are two types of immunity that your body can acquire through exposure to pathogens or antibodies respectively.
They help protect you from infections and diseases but they also have some drawbacks.
Natural Active Immunity: How Your Body Protects You
Often, the immune system needs a “jolt” to get working properly and fight off bacteria, viruses, and other invasions.
Natural active immunity does just that.
It occurs when an individual is exposed to a live pathogen (such as a virus) and develops an immune response.
Fortunately, this form of immunity can protect us from becoming ill from the same disease again in the future.
The primary role of B-cells in natural active immunity is to recognize foreign substances called antigens with special receptors on their surface.
When the B cell recognizes an antigen, it then produces large amounts of antibodies specifically designed to attach themselves to that antigen and help eliminate it from your body.
These antibodies are known as immunoglobulins and they interact directly with cells in tissues to destroy invaders or mark them for destruction by other white blood cells known as macrophages.
In shortᅳB-cells detect dangerous pathogens like viruses or bacteria and then alert the immune system via antibody production so it can rapidly eliminate them.
The primary advantage of natural active immunity comes in its ability to provide long term protection against diseases like measles, chicken pox, rubella, whooping coughs etc.
It also provides swift protection during epidemics or pandemics as it builds up a “herd immunity,” protecting those who haven’t had contact yet with a particular pathogen simply because their environment has become inhospitable for that pathogen due to all around immunization within the populous (this herd effect helps ensure certain diseases remain at bay).
On the downside however, some people could suffer side effects of natural active immunity if the vaccine isn’t manufactured properly.
Make sure you consult with your doctor prior to taking any form of vaccine–natural or otherwise–just so you can be fully prepared for any potential worst case scenario beforehand.
The Adaptive Immune Response: What is it and How Does It Protect Us?
Have you ever wondered about the body’s ability to fight off foreign substances, such as bacteria and viruses? This is known as the adaptive immune response – an incredibly important part of our bodies that works to defend us against diseases.
What is an Adaptive Immune Response?
The adaptive immune system is a component of our overall immunity that can recognize specific molecules of foreign invaders – called antigens – that have entered our body. Once antigens are recognized, B-cells and T-cells work together to neutralize the threat by activating specialized white blood cells, which then secrete antibodies or launch chemical attacks on the invader. Essentially, this response allows us to adapt quickly to changing threats without having prior exposure to them.
Antigen Recognition and Response
First, when an antigen enters your body, it will interact with two types of white blood cells: B cells and T cells. B-cells are responsible for recognizing foreign molecules on the surface of invaders (antigens) and binding with them in order to signal other parts of your body that there is something harmful present.
Upon recognition from B-cells, T-cells will quickly respond by releasing cytokines – signaling proteins that trigger a chain reaction within your body’s defense mechanisms.
Role of B Cells and Antibodies in Adaptive Immunity
Once B-cells recognize an antigen present in the body they will bind with it in order signal your adaptive immunity into action– producing antibodies which circulate throughout your bloodstream looking for any additional foreign bodies they may encounter along their travels.
These antibodies have their own unique shapes that allow them to easily recognize invading antigens so they can bind with them effectively.
These unique shapes also mean they won’t be bound by any normal cells or tissue inside your body– preventing false alarms or accidental destruction of good cells within you.
Role of T Cells in Adaptive Immunity
Once alerted by B-cell activity in response to an antigen presence, T cells are then ready for action. They go about targeting specific infected cells within our body using two core strategies – cytotoxic T cells overwhelm infected cells directly while helper T cells activate other components of our adaptive immunity like macrophage and Natural Killer Cells (NK Cells).
Cytotoxic T Cells are particularly important because they contain small pockets called perforin vesicles filled with toxic compounds designed specifically for destroying pathogens inside our bodies.
They play a key role in overall protection from disease as these toxins prevent viruses from replicating further – meaning infection cannot spread as easily throughout our bodies thus reducing symptoms associated with infections including inflammation, fever, and others.