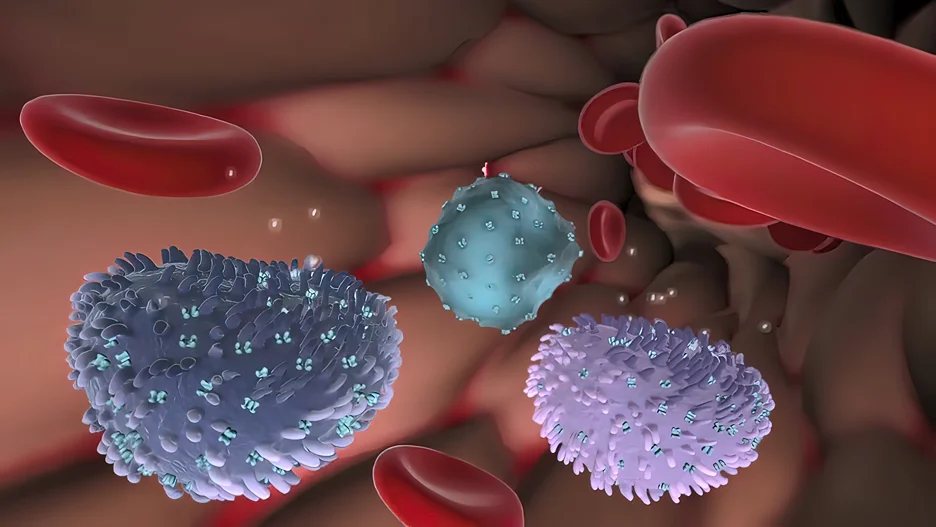
The complement system is a key component of the innate immune system, which serves as the first line of defense against invading pathogens. It is a complex network of proteins that work together to identify and eliminate potential threats to the body.
How the Complement System Connects Innate Immunity and Adaptive Immunity
This system is composed of more than 30 proteins, which are produced by various cells in the body, including liver cells and immune cells. These proteins circulate in the bloodstream and can be activated by a variety of triggers, such as bacterial or viral infections.
When activated, the complement system can trigger a cascade of events that lead to the destruction of invading pathogens. This can occur through several mechanisms, such as opsonization (the coating of pathogens with complement proteins to facilitate their recognition and destruction by immune cells) and the formation of membrane attack complexes (MACs), which can directly lyse the membranes of pathogens.
Role of the Complement System in Host Defense
The complement system is composed of more than 30 proteins that work together to identify and eliminate potential threats to the body. These proteins are produced by various cells in the body, including liver cells and immune cells, and circulate in the bloodstream.
Complement system components
There are three main pathways by which the complement system can be activated: the classical pathway, the alternative pathway, and the lectin pathway. Each pathway is initiated by different triggers but ultimately leads to the same end result – activation of complement proteins that can trigger a cascade of events leading to pathogen elimination.
The complement system can act through several mechanisms to eliminate pathogens. One mechanism involves opsonization, where complement proteins coat pathogens to facilitate their recognition and destruction by immune cells such as macrophages.
Another mechanism involves the formation of membrane attack complexes (MACs), which can directly lyse or destroy pathogen membranes. MACs are formed when certain complement proteins assemble on the surface of invading pathogens, creating a hole in their membrane that causes them to burst.
Complement Pathways and their activation
Classical Pathway
The classical pathway is activated when antibodies bind to antigens on the surface of an invading pathogen. This binding causes a conformational change in the antibody molecule, which allows it to bind to and activate complement protein C1. Activated C1 then activates other complement proteins, ultimately leading to the formation of MACs and opsonization.
Lectin Pathway
The lectin pathway is initiated when certain carbohydrate molecules on the surface of invading pathogens are recognized by mannose-binding lectin (MBL) or ficolins. These molecules then recruit other complement proteins, leading to opsonization and MAC formation.
Alternative Pathway
The alternative pathway is initiated when complement protein C3 spontaneously undergoes hydrolysis in plasma, creating a highly reactive molecule called C3b. C3b can then bind covalently to nearby surfaces, including those of invading pathogens. This binding leads to further recruitment of complement proteins, ultimately resulting in opsonization and MAC formation.
Functions of the complement system
The complement system serves several important functions in the body, including opsonization, chemotaxis, and membrane attack complex (MAC) formation.
Opsonization
Opsonization is the process by which pathogens are coated with complement proteins, making them more recognizable to immune cells such as macrophages and neutrophils. This coating makes it easier for these cells to engulf and destroy the pathogen.
Chemotaxis
Chemotaxis is the process by which immune cells are attracted to sites of infection or tissue damage. Complement proteins can act as chemoattractants, leading immune cells to the site of infection where they can eliminate invading pathogens.
Membrane Attack Complex Formation
Membrane attack complex (MAC) formation involves the assembly of complement proteins on the surface of a pathogen or infected cell, ultimately leading to lysis or destruction of the target cell. The MAC creates a pore in the membrane of the target cell, which causes it to swell and eventually burst.
Complement System’s Impact on Pathogens and Infected Cells
The complement system plays a significant role in identifying and eliminating pathogens and infected cells from the body.
When activated, the complement system can trigger a cascade of events that lead to the destruction of invading pathogens or infected cells. One way this is accomplished is through opsonization of pathogens, which involves coating them with complement proteins that facilitate recognition by immune cells. Once recognized, the immune cells can then engulf and destroy these pathogens.
Another way in which the complement system can eliminate pathogens or infected cells is through membrane attack complex (MAC) formation. MACs are formed when certain complement proteins assemble on the surface of invading pathogens or infected cells, creating a hole in their membrane that causes them to burst.
In addition to directly destroying pathogens and infected cells, the complement system also plays a role in recruiting immune cells to sites of infection or tissue damage through chemotaxis. This process helps to ensure that immune cells are present where they are needed most to fight off infections and promote healing.
Shaping the adaptive immune response
The complement system plays a critical role in shaping the adaptive immune response by linking innate and adaptive immunity.
Link Between Innate and Adaptive Immunity
Innate immunity is the first line of defense against invading pathogens and is composed of various mechanisms, including physical barriers such as skin, mucous membranes, and chemical barriers such as antimicrobial peptides. However, innate immunity alone may not be sufficient to eliminate all pathogens or prevent disease progression.
This is where the complement system comes in. The complement system can help to bridge the gap between innate and adaptive immunity by triggering a variety of responses that can enhance the effectiveness of adaptive immune responses. For example:
- The complement system can facilitate antigen presentation, which involves displaying pathogen fragments to T cells to stimulate their activation.
- Complement proteins can act as chemoattractants for immune cells, bringing them to sites of infection where they can interact with pathogen-specific T cells.
- Complement proteins can also enhance antibody production by B cells, leading to more effective targeting and elimination of invading pathogens.
The link between innate and adaptive immunity is critical for our body’s ability to defend against infections and diseases. The complement system serves as an important mediator between these two systems, helping to enhance their effectiveness and ensure a rapid response to invading pathogens.
Complement System: Role in activating and supporting T cells and B cells
The complement system plays a critical role in activating and supporting T cells and B cells, which are key components of the adaptive immune response.
T cells and B cells are specialized immune cells that help to recognize and eliminate specific pathogens. The complement system can activate these cells by facilitating antigen presentation, enhancing chemotaxis, and promoting antibody production.
Facilitating Antigen Presentation
Antigen presentation is the process by which immune cells display pathogen fragments to T cells to stimulate their activation. The complement system can facilitate this process by opsonizing pathogens with complement proteins, making them more recognizable to immune cells such as dendritic cells. This process helps to ensure that T cells are activated in response to the correct pathogen.
Enhancing Chemotaxis
Chemotaxis is the process by which immune cells are attracted to sites of infection or tissue damage. Complement proteins can act as chemoattractants, leading immune cells such as T cells and B cells to the site of infection where they can interact with pathogen-specific T cells.
Promoting Antibody Production
Complement proteins can also enhance antibody production by B cells, leading to more effective targeting and elimination of invading pathogens. This occurs through several mechanisms, including promoting B cell survival and proliferation, enhancing antigen processing, and increasing antibody affinity.
Complement system in immune surveillance and cancer cells
The complement system is also involved in immune surveillance and plays a role in the recognition and elimination of cancer cells.
Immune surveillance is the process by which the immune system identifies and eliminates abnormal or potentially harmful cells, including cancer cells. The complement system can contribute to this process through several mechanisms.
Opsonization
Complement proteins can opsonize cancer cells, making them more recognizable to immune cells such as macrophages and natural killer (NK) cells. These immune cells can then engulf and destroy the cancerous cells.
MAC Formation
The complement system can also trigger the formation of membrane attack complexes (MACs) on the surface of cancerous cells, leading to lysis or destruction of the target cell.
Regulation of Immune Responses
In addition to directly eliminating cancerous cells, the complement system can also help to regulate immune responses against these cells. For example, complement proteins can interact with T regulatory (Treg) cells, which are specialized immune cells that dampen immune responses. By interacting with these cells, the complement system can help to prevent excessive inflammation and promote immune tolerance against cancerous cells.
Complement deficiencies and disorders
Complement deficiencies and disorders can have a significant impact on the body’s ability to fight off infections and defend against diseases.
Causes and symptoms of complement deficiencies
Complement deficiencies can be caused by genetic mutations or acquired conditions, such as autoimmune diseases. The symptoms of complement deficiencies depend on which components of the complement system are affected and how severe the deficiency is. Some common symptoms may include:
Recurrent Infections
Individuals with complement deficiencies may experience frequent or severe infections, particularly those caused by encapsulated bacteria such as Streptococcus pneumoniae.
Autoimmune Disorders
The complement system plays a critical role in regulating immune responses, and individuals with complement deficiencies may be at increased risk for developing autoimmune disorders such as lupus or rheumatoid arthritis.
Increased Susceptibility to Inflammatory Diseases
Complement deficiencies have been linked to an increased risk for certain inflammatory diseases, such as age-related macular degeneration (AMD) and meningitis.
Delayed Wound Healing
The complement system also plays a role in wound healing, and individuals with complement deficiencies may experience delayed healing or an increased risk of infection at wound sites.
Treatment options and preventive measures
The complement system plays a crucial role in the immune response by identifying and eliminating harmful pathogens, but certain deficiencies or disorders can disrupt this process. When the complement system is not functioning properly, individuals may be more susceptible to infections and autoimmune diseases.
Treatment options for complement deficiencies and disorders vary depending on the specific condition. For example, individuals with hereditary angioedema (HAE) may receive prophylactic therapy with C1 inhibitor concentrate to prevent attacks. In contrast, those with complement protein deficiencies may receive replacement therapy with purified proteins.
Preventive measures can also be taken to reduce the risk of complications associated with complement deficiencies and disorders. These include maintaining good hygiene practices, avoiding exposure to known triggers, such as certain medications or allergens, and following a healthy lifestyle that includes regular exercise and a balanced diet.
It is important for individuals with suspected complement deficiencies or disorders to seek medical attention promptly in order to receive appropriate diagnosis and treatment. With proper management, many individuals are able to lead healthy lives despite their condition.
Frequently Asked Questions
Q: What is complement activation, and how does it contribute to the immune response?
A: Complement activation is the process by which the complement system, a group of proteins in the blood, becomes activated in response to pathogens or foreign substances. This activation triggers a series of reactions, known as the complement cascade, which involves multiple complement components and pathways. Complement activation helps to eliminate pathogens, recruits white blood cells and phagocytic cells to the site of infection, enhances inflammation through the release of inflammatory mediators, and supports the adaptive immune system in mounting a targeted response.
Q: What are the different complement pathways, and how do they interact with one another?
A: There are three primary complement pathways: the classical pathway, the lectin pathway, and the alternative pathway. Each pathway is initiated by different triggers, such as the presence of antibodies, pathogen-associated molecular patterns, or spontaneous hydrolysis of the complement component factor B. While the pathways have distinct initiation mechanisms, they converge at the formation of a key enzyme complex called C3 convertase, which propels the complement cascade forward and leads to the activation of other complement components, such as membrane attack complex formation.
Q: How do complement deficiencies affect the immune system?
A: Complement deficiencies occur when there is a lack or dysfunction of one or more complement components. These deficiencies can weaken the immune system’s ability to fight off infections or remove foreign substances from the body. People with complement deficiencies may be more susceptible to certain bacterial infections and autoimmune diseases. Treatment options may include antibiotic prophylaxis, immunoglobulin replacement therapy, or targeted medications to address specific deficiencies.
Q: What role do NK cells and uninfected cells play in the complement system?
A: Natural killer (NK) cells are a type of white blood cell that can recognize and kill virus-infected cells and cancer cells. While they are not directly involved in the complement system, NK cells can interact with complement components and receptors, enhancing their cytotoxic activity. Uninfected cells, on the other hand, can display complement regulatory proteins, such as factor H, on their cell membranes. This helps protect them from accidental damage by the complement system, ensuring that only harmful pathogens and damaged cells are targeted.
Q: How does the alternative complement pathway differ from the classical and lectin pathways?
A: The alternative complement pathway is unique because it can be activated spontaneously in the presence of pathogens or foreign substances without the need for antibodies or specific pathogen-associated molecular patterns. This spontaneous activation occurs through the hydrolysis of factor B, which binds to complement component C3b, forming the alternative pathway C3 convertase. The alternative pathway serves as a rapid and continuous surveillance system, providing an important first line of defense against infections and contributing to the overall effectiveness of the immune response.
Importance of Understanding the Complement System in Innate Immunity
The complement system is a critical component of the innate immune response, which serves as the body’s first line of defense against invading pathogens. By working in conjunction with other immune cells and molecules, the complement system helps to identify and eliminate harmful microorganisms.
However, when the complement system is not functioning properly, it can lead to significant health problems such as increased susceptibility to infections or autoimmune disorders. Therefore, understanding how this complex system works is essential for maintaining robust immune health.
At SeeBeyond Medical, we are committed to providing comprehensive solutions for immune health that include a focus on enhancing complement system function. Our innovative products are designed to support the body’s natural defenses by promoting healthy immune responses.
We believe that promoting immune health is crucial for overall wellness and quality of life, and we strive to develop cutting-edge therapies that address a range of conditions associated with compromised immunity. Through ongoing research and development efforts, we aim to continue advancing our understanding of the complement system and its role in maintaining optimal health.
Whether you are looking for preventative measures or treatment options for complement deficiencies or disorders, SeeBeyond Medical has the expertise and resources needed to help you achieve your goals.
Contact us today to learn more about our commitment to enhancing immune health through innovative solutions.
